Eagle Biosciences Vitamin D ELISA Kit has been used once again in breakthrough research!
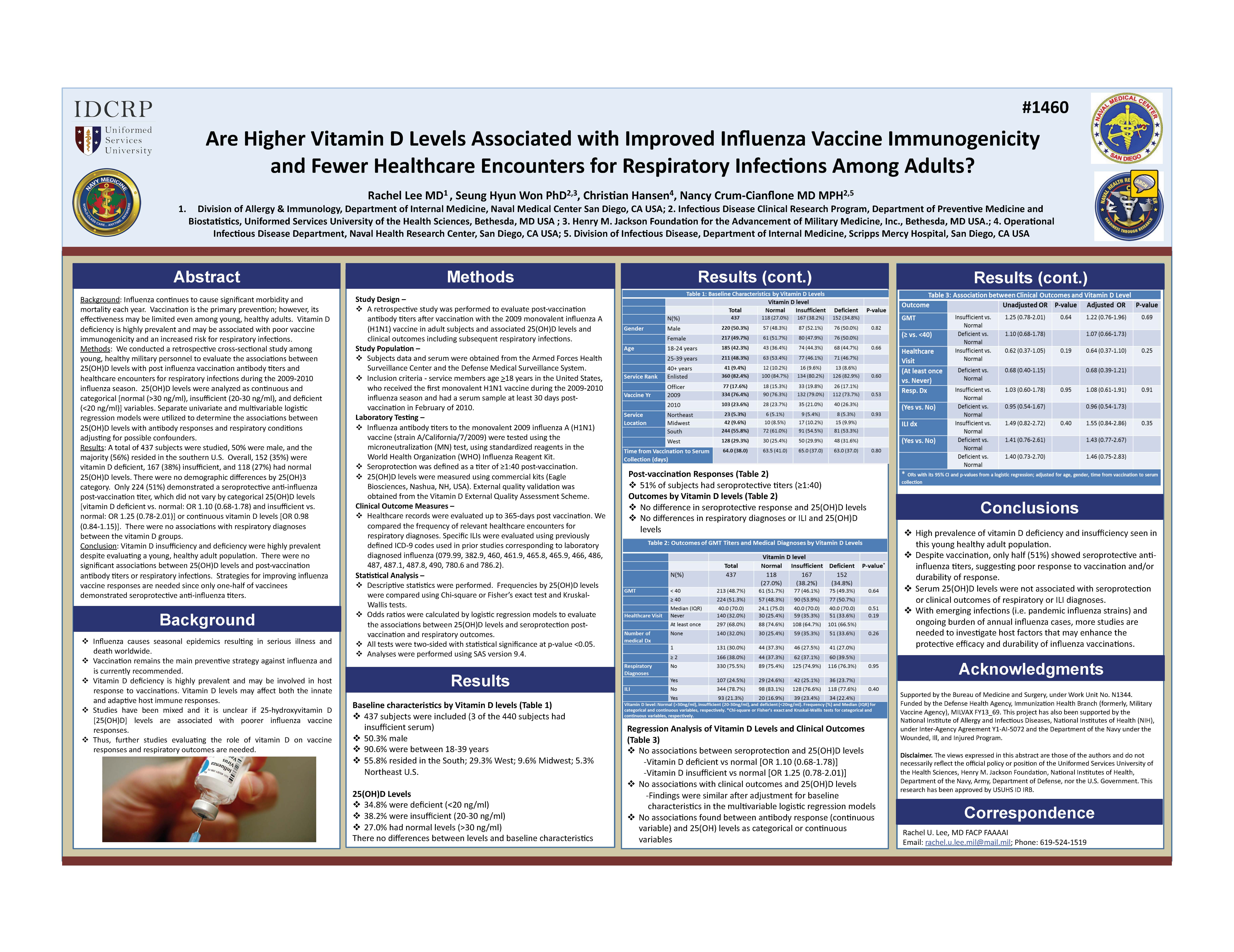
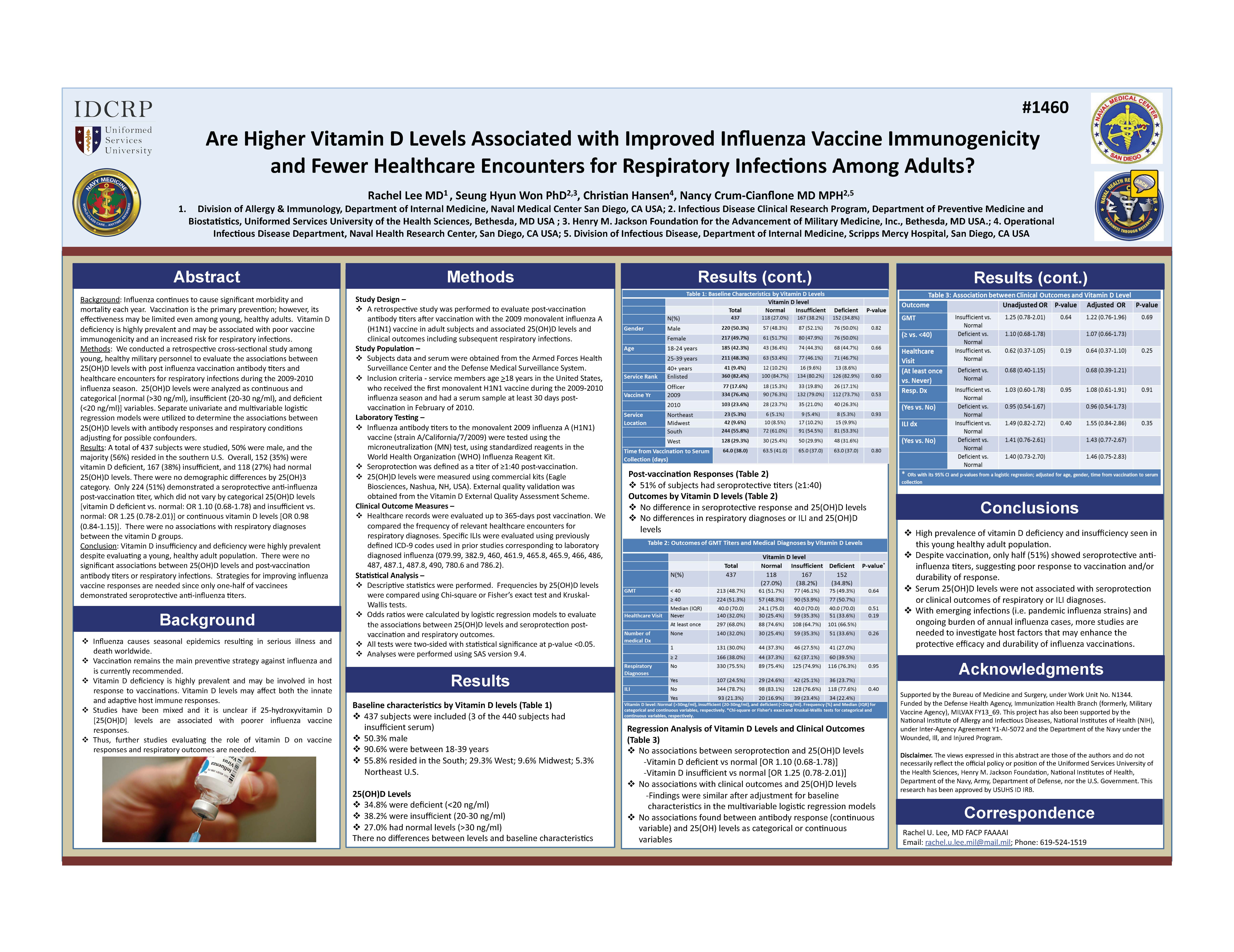
Background: Influenza continues to cause significant morbidity and mortality each year. Vaccination is the primary prevention; however, its effectiveness may be limited even among young, healthy adults. Vitamin D deficiency is highly prevalent and may be associated with poor vaccine immunogenicity and an increased risk for respiratory infections.
Methods: We conducted a retrospective cross-sectional study among young, healthy military personnel to evaluate the associations between 25(OH)D levels with post-influenza vaccination antibody titers (seroprotection defined as a titer of ≥1:40 post-vaccination) and healthcare encounters for respiratory infections during the 2009-2010 influenza season. 25(OH)D levels were analyzed as continuous and categorical [normal (>30 ng/ml), insufficient (20-30 ng/ml), and deficient (<20 ng/ml)] variables. Separate univariate and multivariable logistic regression models were utilized to determine the associations between 25(OH)D levels with antibody responses and respiratory conditions adjusting for possible confounders.
Results: A total of 437 subjects were evaluated. Most participants were young adults (91% were 18-39 years of age), 50% were male, and 56% resided in the southern U.S. Overall, 152 (35%) were vitamin D deficient, 167 (38%) insufficient, and 118 (27%) had normal 25(OH)D levels. There were no demographic differences by 25(OH)3 category. Only 224 (51%) demonstrated a seroprotective anti-influenza post-vaccination titer, which did not vary by categorical 25(OH)D levels [vitamin D deficient vs. normal: OR 1.10 (0.68-1.78) and insufficient vs. normal: OR 1.25 (0.78-2.01)] or continuous vitamin D levels [OR 0.98 (0.84-1.15)]. There were no associations with respiratory diagnoses between the vitamin D groups.
Conclusion: Vitamin D insufficiency and deficiency were highly prevalent despite evaluating a young, healthy adult population. There were no significant associations between 25(OH)D levels and post-vaccination antibody titers or respiratory infections. Strategies for improving influenza vaccine responses are needed since only one-half of vaccinees demonstrated seroprotective anti-influenza titers.
Reference: Rachel Lee, MD1, Seunghyun Won, PhD2,3, Christian Hansen, BS1 and Nancy Crum-Cianflone, MD, MPH2,4,5, (1)Operational Infectious Diseases, Naval Health Res. Ctr., San Diego, CA, (2)Infectious Disease Clinical Research Program, Department of Preventive Medicine and Biostatistics, Uniformed Services University of the Health Sciences, Bethesda, MD, (3)Henry M. Jackson Foundation for the Advancement of Military Medicine, Bethesda, MD, (4)Scripps Mercy Hospital, San Diego, CA, (5)Naval Medical Center San Diego, San Diego, CA